Persistent depressive disorder, also known as dysthymic disorder, is a chronic and often debilitating mood disorder that affects millions of people worldwide. This disorder is characterized by persistent feelings of sadness, hopelessness, and low self-esteem that last for a long period of time, typically two or more years. Although persistent depressive disorder may not be as severe as major depressive disorder, it can still have a significant impact on a person’s daily life and functioning.
Symptoms of Persistent Depressive Disorder
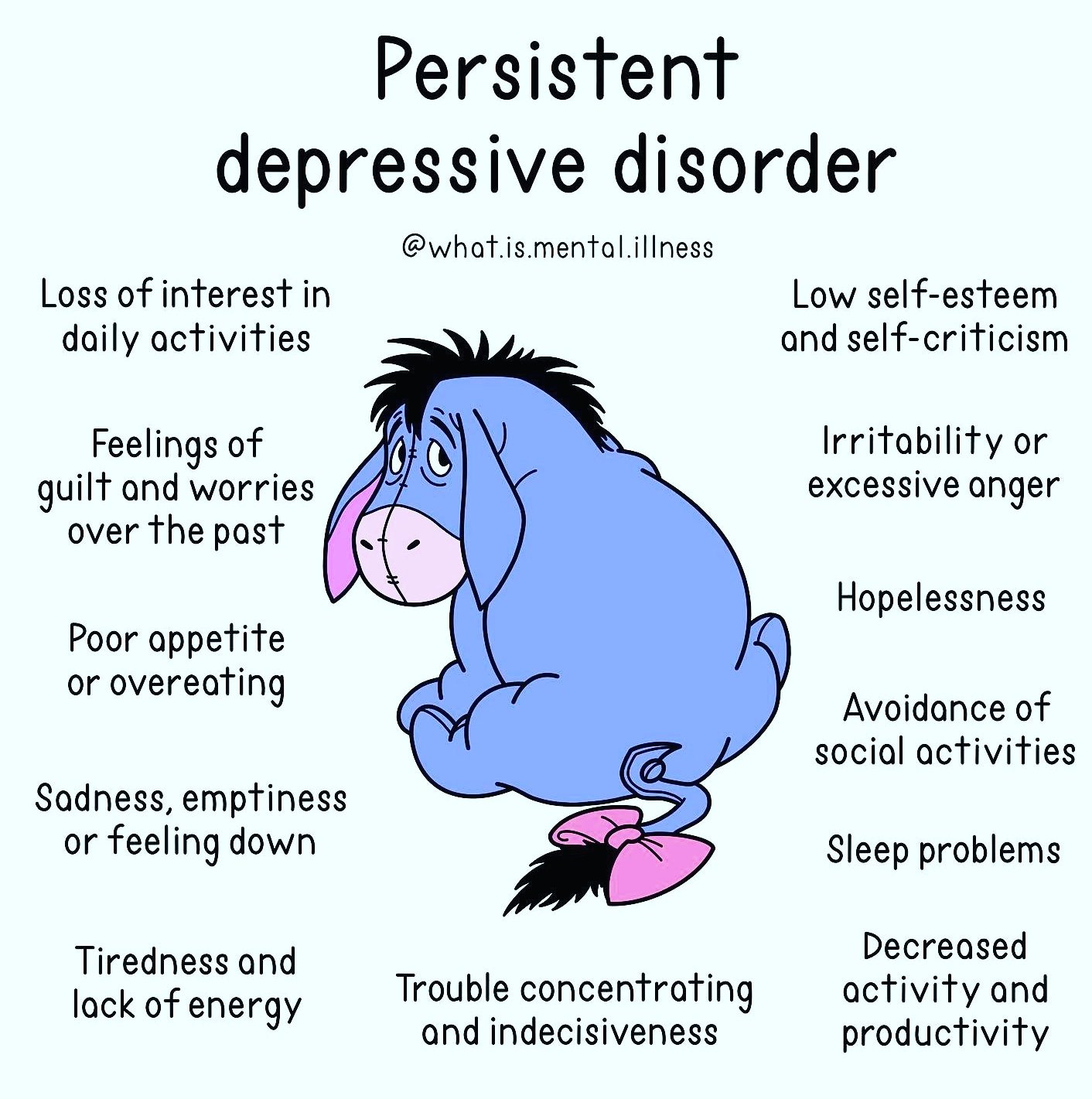
Persistent depressive disorder is diagnosed when a person experiences a depressed mood for most of the day, for more days than not, for at least two years. In addition to feeling sad and hopeless, people with persistent depressive disorder may also experience other symptoms, including:
- Fatigue and lack of energy
- Changes in appetite and weight
- Insomnia or hypersomnia
- Poor concentration or difficulty making decisions
- Feelings of worthlessness or excessive guilt
- Low self-esteem
- Difficulty enjoying activities that were once pleasurable
Causes of Persistent Depressive Disorder
The exact causes of persistent depressive disorder are not yet fully understood. However, there are several factors that are thought to contribute to the development of this disorder. These include:
- Genetics: Like many mental health disorders, persistent depressive disorder may have a genetic component. Studies have shown that people with a family history of depression are more likely to develop the disorder themselves.
- Brain chemistry: Imbalances in certain chemicals in the brain, such as serotonin and norepinephrine, can contribute to the development of persistent depressive disorder.
- Life events: Traumatic life events, such as the death of a loved one, can trigger the onset of persistent depressive disorder in some people.
- Chronic stress: Long-term stress can lead to changes in brain chemistry that increase the risk of developing persistent depressive disorder.
Diagnosis and Treatment of Persistent Depressive Disorder
To diagnose persistent depressive disorder, a mental health professional will typically conduct a thorough assessment of the individual’s symptoms and medical history. This may involve using standardized questionnaires to assess the severity and duration of the person’s symptoms. It is important to note that persistent depressive disorder is often misdiagnosed or underdiagnosed, as people may not seek help for their symptoms or may be unaware that they have a mental health disorder.
Once diagnosed, persistent depressive disorder can be treated in a variety of ways. The most common treatments include psychotherapy, medication, or a combination of both. Cognitive-behavioral therapy (CBT) is one type of psychotherapy that has been shown to be effective in treating persistent depressive disorder. CBT focuses on identifying and changing negative thought patterns that contribute to depressive symptoms. Antidepressant medication, such as selective serotonin reuptake inhibitors (SSRIs), can also be effective in treating persistent depressive disorder. It is important to note that medication should only be prescribed by a qualified healthcare professional and should be closely monitored for potential side effects.
In addition to these traditional treatments, there are several self-help strategies that can be useful for managing persistent depressive disorder. These include:
- Regular exercise: Exercise has been shown to be effective in reducing symptoms of depression and improving overall mood.
- Healthy eating: Eating a balanced and nutritious diet can help improve energy levels and mood.
- Stress management: Learning stress-management techniques, such as meditation or deep breathing, can help reduce chronic stress and improve mood.
- Social support: Maintaining strong social connections and seeking support from friends and family can be helpful for managing symptoms of persistent depressive disorder.
Living with Persistent Depressive Disorder
Living with persistent depressive disorder can be challenging, but it is important to remember that the disorder is treatable.

