Brain stem death, also known as brain death, is a critical condition that occurs when the brain stem, the part of the brain responsible for regulating vital functions such as breathing and heart rate, ceases to function. Brain stem death is irreversible, and it is one of the most profound forms of neurological injury that can occur. This article will discuss the causes, diagnosis, and ethical implications of brain stem death.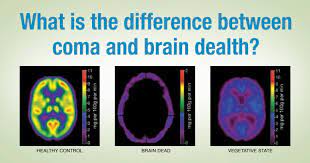
Causes of Brain Stem Death: Brain stem death is typically the result of severe traumatic brain injury, such as a head injury from a car accident or a fall. Other causes can include brain tumours, infections, strokes, and drug overdoses. In these cases, the damage to the brain stem is so severe that it can no longer function properly, resulting in the cessation of vital bodily functions.
Diagnosis of Brain Stem Death :The diagnosis of brain stem death is a complex and highly regulated process. It requires a comprehensive assessment of the patient’s neurological function, which is typically conducted by a team of medical professionals with specialized training in this area. The diagnosis typically involves a series of tests to determine whether the brain stem is functioning, including assessments of the patient’s level of consciousness, brainstem reflexes, and breathing response.
One of the most common tests used to diagnose brain stem death is the apnoea test. This involves removing the patient from mechanical ventilation for a period of time and then assessing whether they are able to breathe spontaneously. If the patient is unable to breathe on their own, this is a strong indicator that the brain stem has ceased functioning.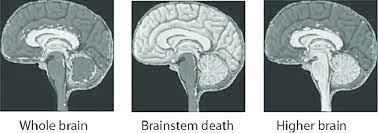
Ethical Implications of Brain Stem Death The diagnosis of brain stem death raises a number of ethical questions, particularly with regard to end-of-life care and organ donation. Because brain stem death is irreversible, patients who are diagnosed with this condition are typically considered to be dead, even if their heart is still beating and their body is being artificially supported through mechanical ventilation.
As a result, decisions regarding the withdrawal of life support and organ donation are typically made following the diagnosis of brain stem death. This can be a difficult and emotional process for families and loved ones, as they must grapple with the fact that their loved one is no longer alive, even though their body may still be warm and their heart may still be beating.
Another ethical issue that arises from brain stem death is the question of how and when to make the diagnosis. In some cases, the diagnosis of brain stem death can take several hours, or even days, to complete. During this time, the patient may be receiving life-sustaining treatments that are both costly and emotionally taxing for their families. On the other hand, if the diagnosis is made too quickly, there is a risk of falsely diagnosing brain stem death and potentially prematurely withdrawing life support.
Brain stem death is a profound and irreversible neurological condition that has significant ethical implications for end-of-life care and organ donation. While the diagnosis of brain stem death is a complex process, it is essential for ensuring that patients receive appropriate care and that their wishes and those of their families are respected. It is important for healthcare professionals to approach the diagnosis and management of brain stem death with sensitivity, empathy, and respect for the dignity of the patient and their loved ones.

